These are procedures in which we use additional energy like radiofrequency waves or laser to stop the blood flow in an abnormal fetus. It is delivered to the fetus by means of a needle inserted into the abnormal baby.
It uses a small needle that is inserted under ultrasound guidance into the tummy of the baby at the site of umbilical cord insertion.
Usually two types of ablation procedures are there-
Ablation procedures are typically utilized in abnormal twin pregnancies. This is usually seen in MONOCHORIONIC TWIN pregnancies- one which in which the babies share their placenta.
The need to perform ablation procedures will be determined by the fetal medicine specialist.
Twin reversed arterial perfusion (TRAP) sequence or acardiac twin is a very rare and unique problem. It is complication seen in approximately 1% of monochorionic twins (twins sharing the placenta).
One twin is structurally completely normal. The other is an abnormal mass of tissue, consisting usually of legs and a lower body, but no upper body, head or heart. Because of the absence of heart, the term acardiac twin is used.
The normal fetus is the “pump twin” because its heart is used to pump blood to the abnormal mass. The acardiac twin has no chance of survival. It receives and pumps back the blood supply from the normal twin via vascular connections present on the surface of the placenta.
The normal twin’s heart has to additional work of pumping the blood to the abnormal one. Due to this the normal twin develops cardiac failure and if nothing is done, then eventually dies.
This is a unique complication seen in Monochorionic pregnancies. Due to presence abnormal vascular communications on the surface of the placenta, one twin acts as pump and the other as recipient. Pump twin pumps blood to the other via these vascular connections. As a result, the pump twin goes small, develops anhydramnios and becomes stuck. The other increases in size, develops polyhydramnios and eventually, cardiac failure. If nothing is done, eventually both the babies die. So, we do laser procedure to ablate these communications or we discuss with the couple for selective reduction of one of the twin, most probably, the stuck twin by means of laser or RFA
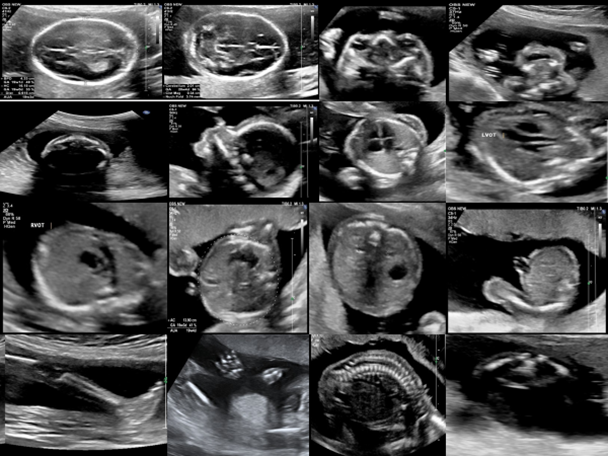
The procedure is performed in the operating room. The procedure is performed under local anaesthesia. First, a detailed ultrasound will be done to confirm the problem, identify the abnormal twin and a pathway for the RFA needle/ spinal needle in laser Local anaesthesia is given into the skin. The needle is inserted into the fetus in the region of umbilical cord insertion. The RFA needle is attached to the RFA generator. If it is laser, then laser fibre is passed through the needle and then connected to the machine producing laser waves. These are then activated until blood flow is stopped in the abnormal twin.Once the procedure is over, the women stays for 24 hours in the hospital.
The success rate is around 80% for these procedures.
There is an increased risk of preterm delivery, leakage of fluid (PPROM) followed by delivery and stoppage of fetal heartbeat of the normal twin. The risk of infection is pretty low.
The shunt procedures are those in which a shunt or a hollow tube is placed through maternal abdomen and uterus into a fluid filled anomaly in the fetus so as to drain the fluid into the amniotic sac.
The commonly done shunt procedures are thoraco-amniotic shunt and vesico-amniotic shunt.
Thoraco- amniotic shunt are done in cases where the baby develops fluid in the thoracic cavity around the heart and the lungs- called as pleural effusion. First by means of 22G needle, the fluid is drained from the thoracic cavity. This fluid is then subjected to number of tests to know the cause. The shunt procedure is considered if there is rapid filling of fluid within the thoracic cavity, mediastinal shift or fluid collections within baby. The shunt drains the fluid in the thoracic cavity into the amniotic sac. The fetal medicine specialist will discuss it with you.
Vesico-amniotic shunt involves placement of shunt through maternal abdomen and uterus into dilated fetal bladder to drain into amniotic fluid. This is done in cases where there is lower urinary tract obstruction (LUTO). There is obstruction at the outlet level of bladder in urethra like posterior urethral valves, urethral atresia or stenosis. Since urine cannot come out properly, it goes back and damages fetal bladder and kidneys as well. LUTO leads to significant perinatal morbidity and mortality. If nothing is done, there will be no proper development of lungs and permanent damage to the kidneys. Ultrasound is done to assess the baby and fluid from the fetal bladder is tested to assess the renal function. The fetal medicine specialist will discuss it with you in detail the findings, pros and cons of the procedure.
The shunt is placed as a last resort so as to decompress the bladder and prevent further damage to the fetal kidneys. The success rate is still controversial.
The risk of these procedures involves shunt migration, closure requiring re-insertion, preterm labour, leakage of amniotic fluid followed by preterm delivery.